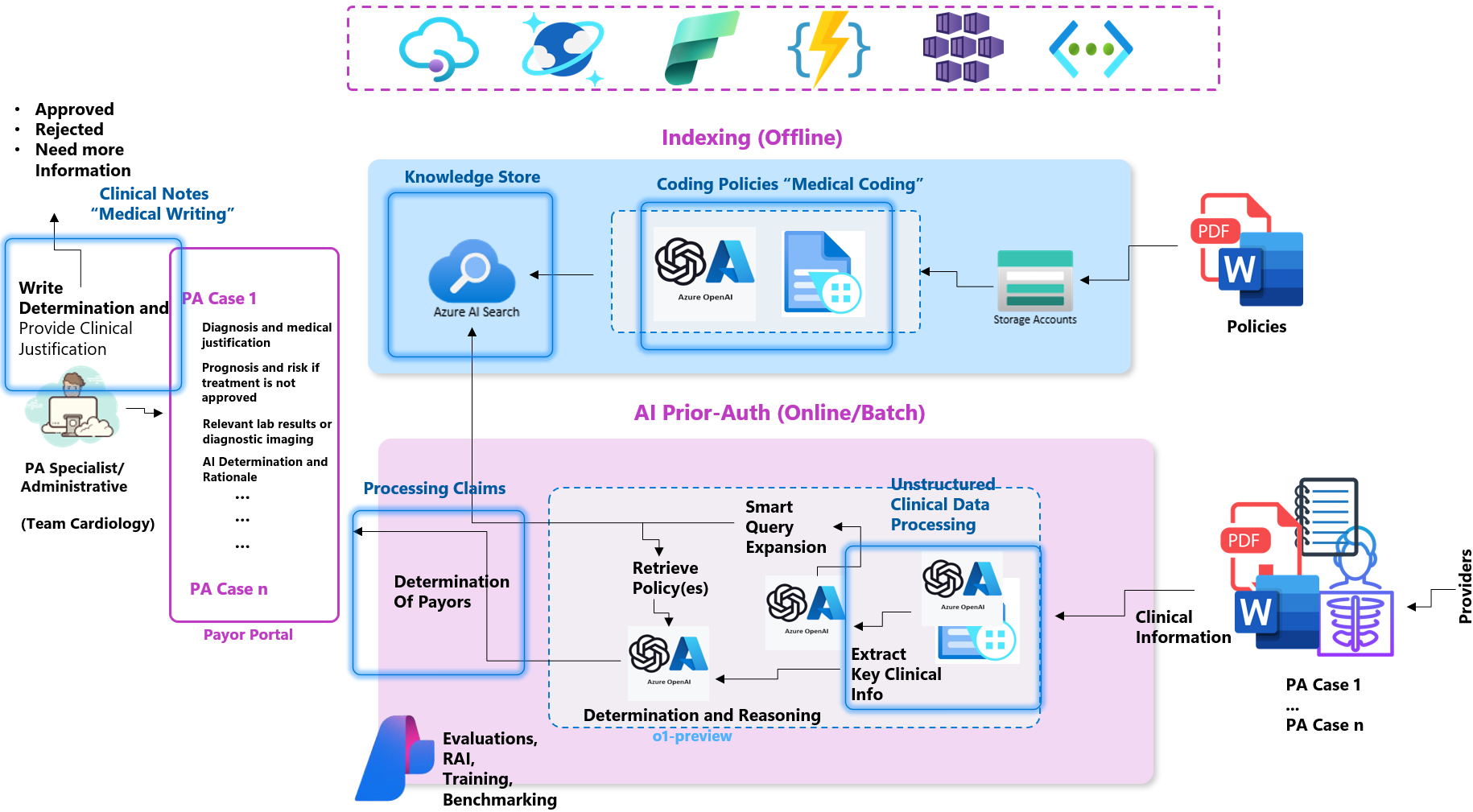
🤖 The AutoAuth Solution
AutoAuth revolutionizes the Prior Authorization (PA) process by integrating cutting-edge AI, advanced Large Language Models (LLMs), and intelligent retrieval systems. This approach minimizes manual workload, accelerates decision-making, and enhances accuracy, all while complying with emerging regulations like CMS 2026 standards.
Core Methodology
- Data Extraction & Structuring
- Use LLM-powered Optical Character Recognition (OCR) and Azure Document Intelligence to convert unstructured data (e.g., PDFs, clinical notes) into structured JSON.
- Extract clinical entities like ICD-10 codes, lab results, and physician notes for precise policy matching.
- Policy Matching & Hybrid Retrieval
- Employ a hybrid approach combining vector-based semantic search and BM25 lexical search via Azure Cognitive Search.
- Dynamically rank and retrieve policy documents that align with case-specific clinical data.
- Reasoning & Decision Support
- Use Azure OpenAI models to assess policies and recommend decisions (Approve, Deny, or Request Additional Information).
- Leverage Semantic Kernel to orchestrate retrieval, reasoning, and decision-making workflows.
Enhanced Capabilities
- LLMOps with AI Studio
- Continuous monitoring, evaluation, and improvement of model performance ensure reliability and scalability.
- Fine-tuned prompts reduce hallucinations and align outcomes with regulatory and clinical guidelines.
- Agentic Retrieval-Augmented Generation (RAG)
- Incorporates agentic pipelines for robust policy matching and reasoning processes.
- Flag missing data or partially met criteria, ensuring decisions are grounded in complete information.
- Transparency & Compliance
- Outputs detailed rationale for each decision, improving auditability and fostering trust between payors and providers.
- Scalable & Configurable Architecture
- Deploy quickly with Azure Bicep templates.
- Modular design ensures easy integration with existing systems and future-ready capabilities.
Key Advantages of AutoAuth
Faster Decision-Making
- Reduces PA turnaround times from days to hours, improving provider and patient satisfaction.
Improved Accuracy
- AI reduces manual errors by up to 75%, ensuring consistent and compliant decisions.
Cost Savings
- Automation cuts processing costs by 40% in high-volume cases, enabling significant operational efficiency for payors.
Patient-Centered Workflow
- Reduces treatment delays, addressing critical healthcare bottlenecks and enhancing patient outcomes.
Phase-by-Phase Workflow
Phase 1: Data Extraction & Structuring
- Converts unstructured data into structured, interoperable formats.
- Identifies key clinical entities like ICD-10 codes, lab results, and physician notes.
Phase 2: Policy Matching & Hybrid Retrieval
- Combines semantic vector-based and lexical search for high-accuracy policy retrieval.
- Dynamically ranks policies based on similarity scores for case alignment.
Phase 3: Advanced Reasoning & Decision Support
- Evaluates compliance with policy criteria using advanced reasoning models.
- Generates transparent decisions with detailed rationales for providers and payors.
CMS 2026 Alignment
AutoAuth is built to align with CMS regulations by enabling:
- Real-Time Data Exchange: Integration with APIs based on HL7 FHIR standards ensures timely responses.
- Transparency in Decision-Making: Outputs include clear reasons for approval or denial, fostering trust and reducing disputes.
Technical Highlights
- Azure OpenAI Service: Models like ‘o1` enable industry-leading context-rich reasoning.
- Azure Cognitive Search: Hybrid search architecture ensures precise policy matching.
- Semantic Kernel Integration: Orchestrates multi-step retrieval and decision workflows.
- Azure Document Intelligence: High-fidelity OCR for unstructured clinical data.
By uniting these components, AutoAuth transforms PA into a faster, more efficient, and patient-centered workflow.